Healthcare Risk and Compliance: 5 Key Challenges to Address in 2025
- GRC
- 18 July 24
Introduction
Healthcare is one of the most strictly regulated sectors in the world. This is understandable and necessary considering that the sector deals with factors as crucial and sensitive as health and life itself. As a result, this sector has witnessed increasing regulatory complexity with different regulatory bodies focusing on various aspects of the industry. The healthcare business is also rapidly evolving and expanding with many providers offering ancillary services such as health insurance and insuretech. This makes the sector susceptible to various new and emerging risks. Healthcare providers also work with third parties who handle sensitive patient information, making it vital for them to effectively manage third-party risks. As regulatory complexity increases amidst a fraught risk landscape, ensuring compliance can be challenging.
In April 2024, records of 13.4 million patients were left exposed thanks to nine incidents of unauthorized access or disclosure of protected health information. 44 hacking incidents in the same month affected 1,919,637 records. The consequences of such breaches through penalties and impact on reputation and image are significant. This blog explores the top five risk and compliance challenges for the healthcare sector and how to address them.
What Are Compliance Issues in Healthcare?
Healthcare Compliance Issues refer to instances where healthcare organizations fail to adhere to relevant laws, regulations, and industry standards. Non-compliance can lead to severe consequences, including fines, penalties, legal actions, and reputational damage.
1. Regulatory Compliance
The healthcare sector is governed by regulations and frameworks such as Health Insurance Portability and Accountability Act (HIPAA), the HITECH Act that complements HIPAA by increasing the penalties for data breaches, the 21st Century Cures Act, General Data Protection Regulation (GDPR), PCI DSS, California Consumer Privacy Act (CCPA), Health Information Trust Alliance Common Security Framework (HITRUST CSF), Information Blocking Rule (2021) and Interoperability and Patient Access Final Rule (2021). Most of these focus on patient data privacy, data security, access to information, and cyber security.
Each of these is constantly being updated to keep pace with a rapidly changing risk landscape. For example, this year HIPAA saw some significant updates to its patient privacy provisions and outlined stricter cyber security requirements. It gives patients greater control over their data and mandated risk assessments, incident response plans, data encryption requirements, and updated breach notification requirements. Keeping pace with these updates, assessing their impact on various processes and functions, and adapting internal controls and policies is a significant challenge.
Furthermore, there are federal, state, and local regulations and rules that apply to healthcare providers. Each state has specific reporting requirements regarding public health emergencies, infectious disease outbreaks, and specifying how long medical records can be retained. Some states may even have their own laws regarding patient data. For example, California has laws pertaining to data breach notifications that have to be complied with in addition to HIPAA. Healthcare providers must report relevant situations to their state or local agencies in the prescribed format in addition to complying with federal regulations.
Additionally, healthcare providers must be accredited by industry organizations such as The Joint Commission (TJC) that evaluates organizations on parameters such as patient care safety and healthcare management, Accreditation Association for Ambulatory Health Care (AAAHC), and Urgent Care Association (UCA). This shows that the provider meets quality and safety benchmarks set by the governing bodies. Meeting accreditation requirements, and complying with standards set by each of these bodies is a complex and challenging task.
2. Enterprise Risk and Incident Management
Healthcare providers have to efficiently manage risks unique to the sector, in compliance with the relevant regulations. In addition to compliance risks, healthcare providers have to be prepared to deal with risks related to patient care and safety as any lapses can have severe legal and financial impacts in addition to damaging reputation and trust. They must be cognizant of risks pertaining to medical instruments and devices in the form of potential malfunctions that impact patient care. There are also risks pertaining to insurance claims, frauds, phantom billing, and upcoding. They have to conduct risk assessments periodically to identify and mitigate potential compliance issues and threats. They also must have comprehensive incident management processes in place to report and respond to crises quickly and effectively. Risks ranging from business operations, third parties, cybersecurity, ESG, and health hazards must be managed effectively along with appropriate business continuity plans. The healthcare industry must move from compliance check-in-the-box activity to proactive risk management to thrive in the complex risk landscape.
3. Data Privacy and Cyber Security
Patient healthcare data and records are sensitive and subject to strict security, privacy, and protection laws. Healthcare providers have to ensure that their technology systems meet HIPAA standards, which may prove to be a daunting exercise, particularly for smaller organizations.
Regulations like the 21st Century Cures Act emphasize the need for seamless and secure data sharing. And so, organizations must ensure their electronic health record systems are updated, secured, compliant with regulatory standards, and capable of securely executing data exchanges. It is equally important to ensure that different healthcare systems are interoperable while maintaining data security and privacy. Organizations must also ensure that their technology systems are updated and compliant with the latest security and regulatory standards to protect patient information and ensure foolproof compliance.
Adding to the challenge is the fact that the threat landscape is continually evolving with bad actors increasingly leveraging advanced technology to launch sophisticated attacks. Protecting health care data under these conditions can be a Herculean task. In February 2024 alone there were 24 data breaches, the biggest of which was the breach at Medical Management Resource Group that compromised 2.35 million records. Hacking and ransomware continue to plague the sector and only four breaches affecting 10,000 or more records in February were not hacking incidents. Data encryption is important to protect healthcare records. But ensuring encryption both in transit and at rest to prevent unauthorised access is a challenge.
The rapid evolution of Artificial Intelligence technologies has the potential to transform healthcare. From early detection, faster diagnoses, and better treatment to improved monitoring, decision-making, research, and training, AI is already being leveraged to drive better healthcare outcomes. But, AI comes with a significant risk of data breaches. AI platforms process huge volumes of sensitive data and any vulnerabilities can be exploited by bad actors. Healthcare providers leveraging AI must be cognizant of the security risks associated with it and implement stringent data protection strategies.
4. Third-Party Risk Management
Healthcare organizations rely on numerous external vendors ranging from cloud service providers to billing companies, medical device manufacturers and suppliers, and more. Many of these have access to sensitive healthcare data and are subject to the standards set by HIPAA. This is also a vulnerability that can be targeted by hackers. Additionally, healthcare providers must monitor third parties for operational and ethical risks as well as such unavailability or disruptions to medical services, AML, bribery, and other malpractices. Third-party organizations are subject to data protection and privacy regulations such as GDPR and PCI DSS. Healthcare providers must monitor their partners’ compliance with all relevant regulations, as well as their overall risk management and mitigation strategies.
Managing third-party risk must be a crucial part of a healthcare organization’s risk management strategy. They must conduct regular due diligence with vendor risk assessments and security assessments. Compliance with all relevant regulations and standards, and risk evaluation must be a contractual obligation for all third-party vendors working with healthcare organizations. In fact, the HITECH ACT extends HIPAA’s regulations to vendors and includes penalties for vendors for non-compliance. Healthcare organizations must regularly monitor their partners and conduct comprehensive and periodic audits to ensure ongoing compliance. Establishing BAAs with vendors to ensure compliance with a wide range of regulations is advisable, but managing third-party risks adds to the significant compliance challenges of healthcare organizations.
5. Continuous Monitoring and Reporting
Healthcare providers are operating within a regulatory landscape that is continuously evolving and they must ensure error-free compliance. They have to monitor the regulatory landscape on an ongoing basis to keep pace with emerging regulations and have the capability to adapt and map new regulations and updates to existing practices and controls. Continuous and automated monitoring of risks and controls is crucial for enabling real-time risk assessments, quick decision making, and faster, more effective mitigation efforts. They must have rationalized internal controls to mitigate risks and ensure compliance. They must have automated processes to onboard new third parties and carry out due diligence to ensure there are no gaps in compliance. They must also conduct regular digitized audits and continuous monitoring of compliance processes to ensure there are no gaps. Maintaining compliance reports, logs of security events and communicating with regulatory authorities is another key task for organizations.
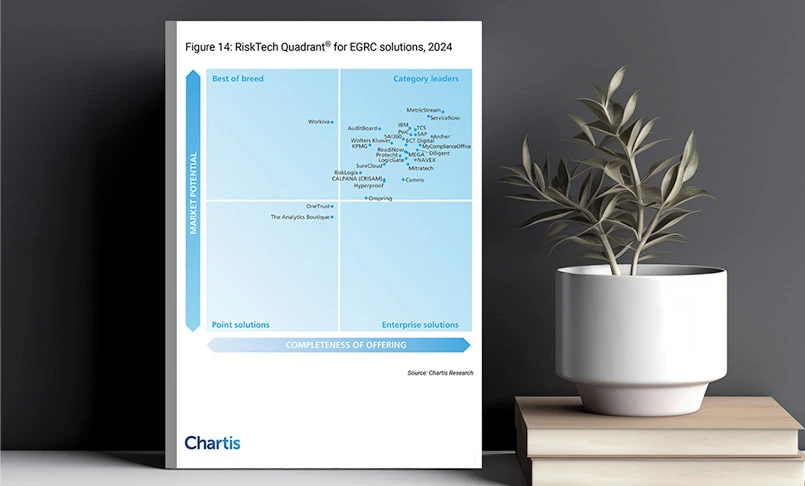
Power-Up Your GRC Program with MetricStream
MetricStream’s Healthcare solution is purpose-built to help organizations in this highly regulated industry adopt and implement a streamlined, automated, and integrated approach to GRC. Healthcare providers can leverage advanced capabilities for managing regulatory compliance, enterprise risks, including cyber and third-party risk, and internal audit, to improve their overall risk and compliance posture and drive better-informed decision-making.
With MetricStream, your organizations can effectively:
- Improve risk visibility with faster response to perceived risks, automate capture and management of regulatory changes
- Streamline and digitalize GRC activities across the three lines of defense
- Enhance cyber resilience with 360-degree visibility into cyber risks, threats, vulnerabilities, risk exposures, and compliance violations
- Simplify and improve third-party risk management with automated processes for onboarding, real-time monitoring and control assessments
- Prioritize internal audits with risk-based audits and automate audit reporting
Interested to find out more? Request a demo now.